Is There a Link Between a Deviated Septum and Sleep Apnea?
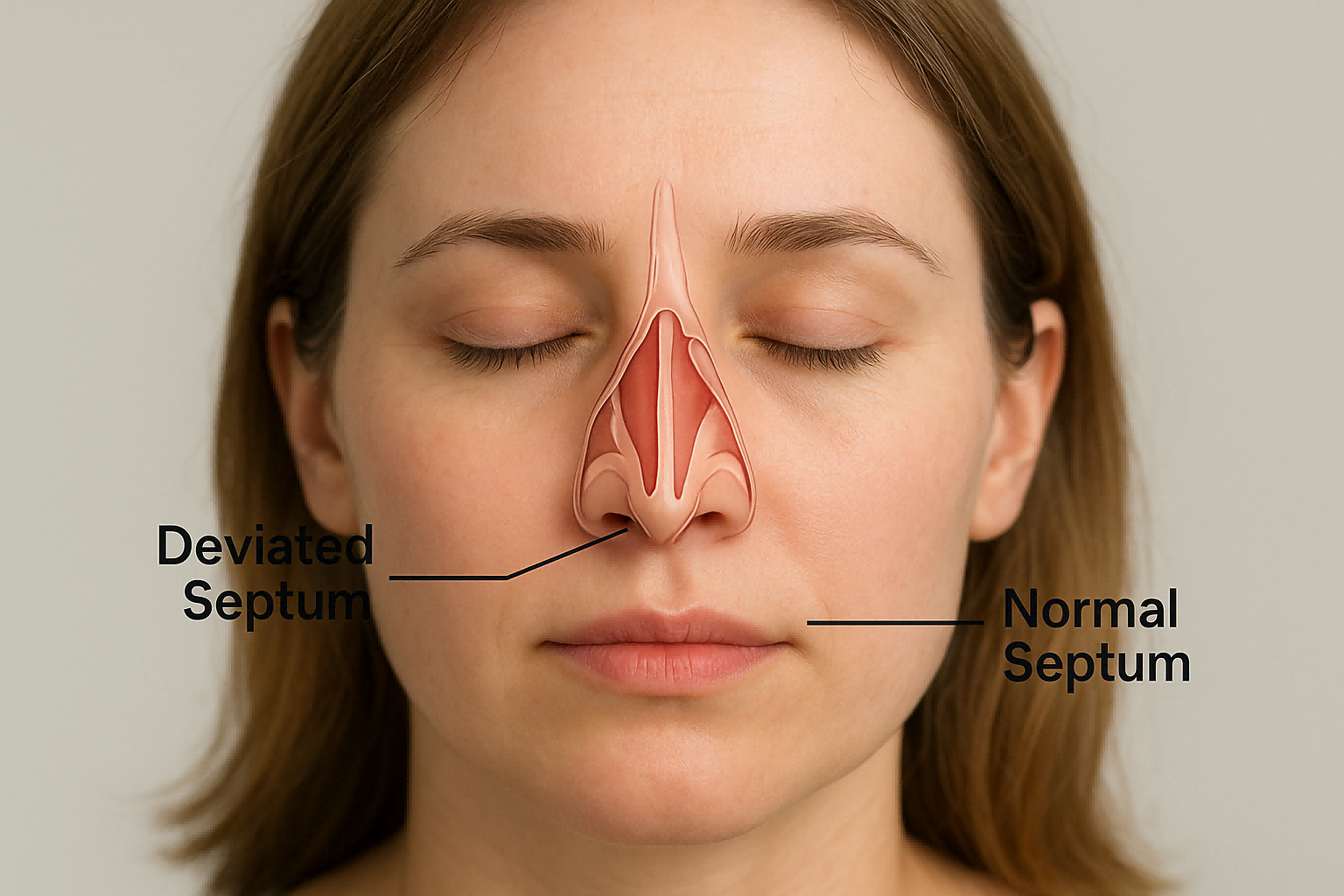
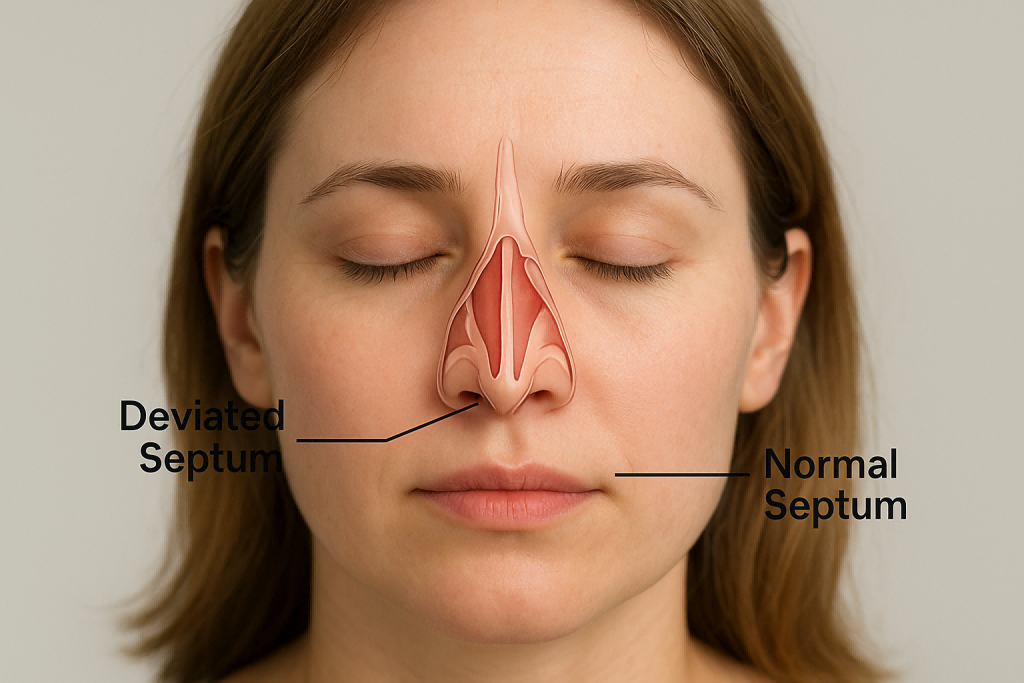
What is a Deviated Septum?
A deviated septum occurs when the thin wall of cartilage and bone dividing your nostrils is displaced to one side. Ideally, the septum should be straight and centered, allowing equal airflow through both nostrils. However, in many people, the septum leans slightly to the left or right. When this deviation is significant, it can cause airflow obstruction, breathing difficulties, and other health issues.
Causes of a Deviated Septum
Several factors can lead to a deviated septum:
- Congenital condition: Some people are born with a crooked septum.
- Injury or trauma: A blow to the nose during sports, accidents, or fights can cause deviation.
- Developmental changes: The septum may shift during growth spurts in adolescence.
Common Symptoms and Complications
Symptoms of a deviated septum can vary. Some people hardly notice it, while others experience:
- Chronic nasal congestion
- Frequent nosebleeds
- Sinus infections
- Headaches due to sinus pressure
- Difficulty breathing, especially during physical activity or sleep
When left untreated, a deviated septum can worsen snoring and may contribute to sleep-disordered breathing.
What is Sleep Apnea?
Types of Sleep Apnea
Sleep apnea is a disorder characterized by repeated pauses in breathing during sleep. The main types include:
- Obstructive Sleep Apnea (OSA): Caused by airway blockages, often due to soft tissue collapse or nasal obstruction.
- Central Sleep Apnea (CSA): Caused by the brain’s failure to send signals to breathing muscles.
- Complex Sleep Apnea Syndrome: A combination of both OSA and CSA.
Key Symptoms of Sleep Apnea
Some of the most noticeable symptoms are:
- Loud snoring
- Gasping or choking during sleep
- Morning headaches
- Daytime sleepiness and fatigue
- Difficulty concentrating
Risk Factors and Long-Term Health Impact
Risk factors include obesity, smoking, family history, and nasal abnormalities. If left untreated, sleep apnea increases the risk of heart disease, stroke, diabetes, and hypertension.
The Connection Between Deviated Septum and Sleep Apnea
How Nasal Blockages Affect Breathing During Sleep
A deviated septum can make it harder for air to flow through the nasal passages. When breathing becomes obstructed, especially at night, the body struggles to get enough oxygen, potentially triggering or worsening obstructive sleep apnea.
Scientific Evidence Linking the Two Conditions
Studies suggest that people with a deviated septum have a higher likelihood of developing OSA. However, while nasal obstruction contributes to poor sleep, it’s not always the sole cause of apnea. Other factors—like obesity or soft palate collapse—also play significant roles.
Misconceptions About Deviated Septum and Sleep Apnea
It’s important to note that not everyone with a deviated septum has sleep apnea, and not every case of sleep apnea is caused by nasal obstruction. The relationship is often complex and influenced by multiple risk factors.
Diagnosing Deviated Septum and Sleep Apnea
Medical Evaluation and Tests
A deviated septum can usually be diagnosed during a routine ENT (ear, nose, and throat) examination. The doctor may use a nasal speculum or an endoscope to look inside your nose. For sleep apnea, however, a more comprehensive evaluation is needed.
Role of Polysomnography (Sleep Study)
A sleep study (polysomnography) is the gold standard for diagnosing sleep apnea. It records breathing patterns, oxygen levels, heart rate, and brain activity during sleep. If you have both a deviated septum and suspected sleep apnea, your doctor might recommend this test to see how much the nasal obstruction contributes to your sleep issues.
When to See a Specialist
If you experience persistent nasal congestion, loud snoring, or daytime fatigue, it’s wise to consult both an ENT and a sleep specialist. Early diagnosis can prevent complications and improve quality of life.
Treatment Options for Deviated Septum
Non-Surgical Management (Nasal Strips, Sprays, Lifestyle)
Not every deviated septum needs surgery. Mild cases can often be managed with:
- Nasal dilator strips to widen the nostrils.
- Decongestant sprays or antihistamines to reduce swelling.
- Saline sprays to keep nasal passages moist.
- Lifestyle changes like avoiding allergens and sleeping on your side.
Surgical Treatment: Septoplasty and Rhinoplasty
For severe deviations, septoplasty (a surgical procedure to straighten the septum) is often recommended. Sometimes it’s combined with rhinoplasty (reshaping the nose) to improve both function and appearance. Surgery can significantly improve airflow, reduce snoring, and enhance overall sleep quality.
Treatment Options for Sleep Apnea
CPAP and BiPAP Therapy
The most common treatment for moderate to severe sleep apnea is Continuous Positive Airway Pressure (CPAP). This machine delivers pressurized air through a mask to keep the airway open. For some patients, BiPAP (bi-level positive airway pressure) may be used as an alternative.
Oral Appliances and Lifestyle Modifications
Custom oral appliances can reposition the jaw and tongue to prevent airway collapse. Lifestyle changes, such as weight loss, reducing alcohol intake, and quitting smoking, also play an important role in managing apnea.
Surgical Interventions for Severe Cases
When conservative treatments fail, surgical procedures—such as uvulopalatopharyngoplasty (UPPP) or maxillomandibular advancement—may be considered. These surgeries widen the airway to reduce apnea episodes.
Can Septoplasty Improve Sleep Apnea Symptoms?
Research Findings on Surgical Outcomes
Research shows mixed results. While septoplasty alone may not cure sleep apnea, it can reduce nasal resistance, making CPAP therapy more effective and comfortable. Many patients report fewer breathing interruptions after surgery, especially when nasal obstruction was a major contributing factor.
Patient Experiences and Success Rates
Patients with both a deviated septum and mild OSA often notice improvement in snoring and breathing after surgery. However, those with severe OSA usually require a combination of treatments, not just septoplasty.
Lifestyle Tips to Improve Sleep Quality with Deviated Septum
Sleeping Positions and Nasal Breathing Exercises
- Side sleeping reduces airway collapse compared to sleeping on your back.
- Nasal breathing exercises, such as alternate nostril breathing, can strengthen airflow.
- Using a humidifier keeps nasal passages moist, easing congestion.
Diet, Weight Management, and Sleep Hygiene
- Maintain a healthy weight, since excess fat can worsen sleep apnea.
- Avoid heavy meals, alcohol, and sedatives before bed.
- Stick to a consistent sleep schedule and create a calming bedtime routine.
FAQs About Deviated Septum and Sleep Apnea
1. Can a deviated septum cause sleep apnea directly?
Not always. A deviated septum can contribute to nasal obstruction, which worsens sleep apnea, but it’s rarely the sole cause.
2. Will fixing my deviated septum cure sleep apnea?
Septoplasty may improve symptoms, but most patients still require other treatments like CPAP.
3. How do I know if my snoring is due to a deviated septum?
If one nostril feels consistently blocked, and you snore loudly, a deviated septum could be contributing. An ENT evaluation can confirm it.
4. Can sleep apnea get worse over time if untreated?
Yes, untreated sleep apnea can lead to high blood pressure, heart disease, and other serious health issues.
5. Is septoplasty a painful surgery?
Most patients report mild to moderate discomfort after septoplasty, with full recovery in 1–2 weeks.
6. Can children have sleep apnea from a deviated septum?
Yes, but it’s less common. Enlarged tonsils and adenoids are usually the main cause of pediatric sleep apnea.
Conclusion: The Link Between a Deviated Septum and Sleep Apnea
So, is there a link between a deviated septum and sleep apnea? The answer is yes—nasal obstruction from a deviated septum can contribute to or worsen sleep apnea, but it’s usually not the only factor. Treatments like septoplasty, CPAP therapy, and lifestyle modifications often work best when combined.
If you suspect you have either condition, consult a doctor early. A personalized treatment plan can help you breathe easier, sleep better, and live healthier.
🔗 For more detailed research on sleep apnea, visit American Sleep Apnea Association.